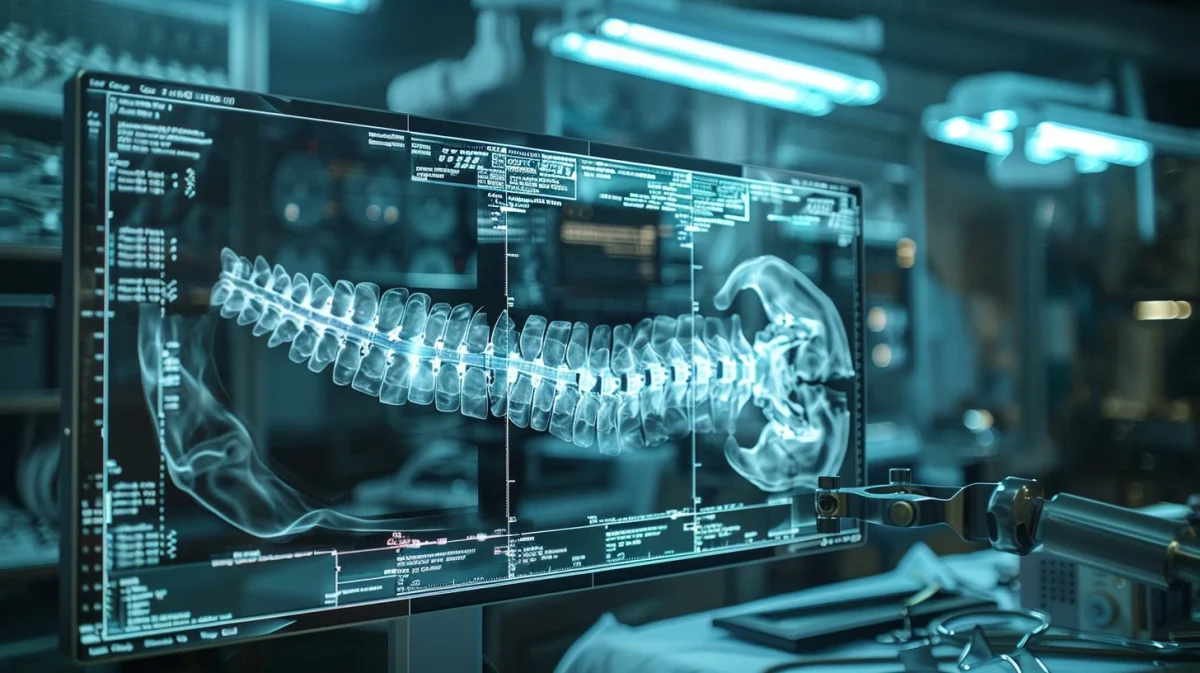
Besides general important advantages that one may deem worthy, personalized medicine may show great promise to be far more effective than the traditional approaches. AI has the ability to integrate multi-omics data, which will be able to analyze extremely diverse datasets, including genetic, clinical, and lifestyle data. A simple way to define multi-omics data would be the general data that is generated from the genome, proteome, transcriptome, metabolome, and epigenome. This data will help identify personalized treatment options based on the patient’s individual profiles. This comprehensive analysis allows for a far more holistic understanding of disease mechanisms and treatment responses and allows for a better overall decision about what is best for the patient.
In addition to this, AI algorithms can predict the patient’s responses to specific treatments and drugs by learning from large datasets of patient outcomes and biomarker profiles. As well as using the individual’s data, the algorithms could source similar patient’s and analyze what was the most effective for them. This predictive modeling will enable clinicians to almost tailor treatments to individual patients, therefore optimizing efficacy and minimizing adverse effects. This data may also be used to identify individuals at high risk of developing certain diseases or conditions. This early detection has the ability to save lives or lengthen life spans due to its ability to enable proactive intervention. These interventions could include lifestyle modifications, preventive treatments, or much-needed procedures to reduce the likelihood of disease onset or its progression.
These treatments will be patient-specific as the AI algorithms can analyze their data, such as genetic variations, biomarker profiles, and treatment responses, to make sure the most effective treatments are used for the patient, especially for those with malignant diseases such as cancer. With the use of personalized medicine, the aim is to minimize the risk of adverse drug reactions by deeply considering each individual patient’s characteristics, such as their genetic predispositions and comorbidities, when prescribing medications. This cautious approach of drug selection and dosing strategies will improve the outcome greatly.
In addition, personalized medicine encourages a patient’s active involvement and participation in the process of their healthcare decisions by providing them with personalized treatment options and insights into their health risks and outcomes. The transparency, personalization, and options of this approach allow the patient to be more aware of the situation and knowledgeable of the best course of action in order to have the most effective and successful treatment. This increased engagement fosters a collaborative relationship between the patients and their healthcare providers, leading to far better treatment adherence and long-term health management.
Another significant factor is the cost-effectiveness of optimizing treatment selection and avoiding unnecessary interventions with personalized medicine through AI algorithms. It has the potential to reduce healthcare costs associated with ineffective or unneeded treatments, hospitalizations, and adverse events, as the prices of these may be very costly. An AI-driven predictive modeling algorithm can help identify the most cost-effective interventions and allocate healthcare resources more efficiently. Healthcare professionals, hospitals, and any other medical-related institution should focus all of their attention on patients who need their assistance rather than patients being in a hospital bed for no real reason.
This efficient method of allocating and allowing only patients who really need the attention of a medical professional may save countless lives. The collected data enables AI to analyze large-scale patient data to identify novel disease subtypes, biomarkers, and therapeutic targets. This data-driven approach will massively accelerate biomedical research and drug development by precisely guiding the design of clinical trials, identifying patient populations for targeted therapies, and facilitating the discovery of new drug candidates.
However, challenges and limitations arise associated with AI algorithms in personalized medicine. Similar to other departments in which AI is likely to be used, the quality, completeness, and accuracy of the data are critical for a successful use. Unfortunately, understanding the thought process of an algorithm is extremely difficult and therefore making their data and opinions susceptible to errors and questions. This is due to the artificial intelligence being taught by human data, which can lead to human complications such as bias. These errors and biases can lead to incorrect predictions in a patient’s treatment recommendations, emphasizing just how important data quality control and validation are. Any data collected and provided by these algorithms should be heavily tested and studied before put into use.
The difficulty of interpreting AI-generated recommendations and ideas will require overcoming various logistical and regulatory hurdles. Clinicians will likely require training in order to understand artificial intelligence, and regulatory agencies may need to establish guidelines for the validation and approval of AI-driven diagnostic and treatment tools. These guidelines will very likely be far more strict than their human counterpart. Furthermore, the thought of AI collecting and analyzing personal data and using it on a large web raises many ethical and privacy concerns related to patient consent, data security, and the potential misuse of sensitive health information.
When any new innovation comes to life and interacts with the population, the result is a large amount of skepticism and very little trust for the invention. It will most likely take years or even decades for the majority of people to feel comfortable with the use of AI in personal data. To ensure that this even happens eventually, patient autonomy, confidentiality, and data protection will be essential to maintain trust and ethical integrity in the practice of AI-driven personalized medicine. As artificial intelligence is a relatively new part of technology and is extremely sophisticated, access to these benefits may be heavily limited by socioeconomic factors, geographic location, and disparities in healthcare access. Addressing these issues is crucial to ensure that personalized treatments are accessible to all patients, regardless of their background, circumstances, or previous history. The ultimate question remains: will my insurance cover AI?
Despite these challenges and the difficult task of overcoming them, artificial intelligence shows strong potential to revolutionize personalized medicine by enabling extremely precise diagnosis, treatment selection, and monitoring, ultimately leading to more positive health outcomes for individual patients. AI will not be able to do this alone, rather, the collaborative efforts between itself, researchers, clinicians, policymakers, and even the patients are essential in order to best address these challenges and unlock the full potential of AI in personalized medicine the most effectively and efficiently.
Overall, personalized medicine empowered by artificial intelligence holds tremendous promise for the many topics stated in this post. As technology continues to evolve and our understanding of disease mechanisms deepens, personalized medicine will play an increasingly central role in ushering in a new era of delivering precision healthcare specifically tailored to the individual needs of each patient.